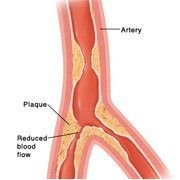
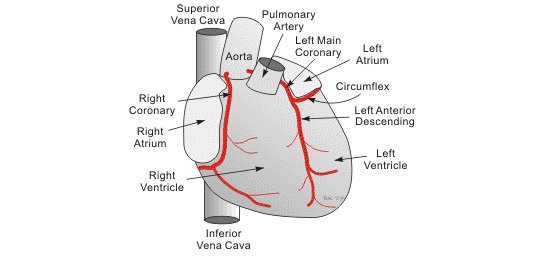
The sequence of events after the onset of myocardial ischemia is known as the ischemic cascade. Early left ventricular dysfunction is a characteristic, which in itself may cause a further fall in coronary blood flow. A vicious cycle is set up where increasing heart rate and blood pressure raises myocardial demand, and shortened diastolic times reduce coronary blood flow. Recurrent episodes of ischemia lead to adaptive changes in myocardial metabolism and “hibernation”, resulting in chronic but potentially reversible left ventricular dysfunction.
Modifiable Risk Factors
Risk factors for atheromatous disease that are modifiable (present in almost 50 per cent of patients) include smoking, hypertension, high cholesterol and diabetes mellitus. Of these, smoking is by far the most important, (see: how to quit smoking). Although cholesterol levels are significantly higher in patients with angina compared to others, there is considerable overlap between the groups. In about 80 per cent of patients with Angina Pectoris, cholesterol is within the normal range, as defined by controls.
Related Links
- Simple Definition of Angina Pectoris
- Signs and Symptoms of Angina Pectoris
- How To Diagnose and Investigate Angina Pectoris?
- Useful Tips on The Management of Angina Pectoris
Leave A Comment